RCM Offerings
Personalized Healthcare Revenue Cycle Solutions
Our offerings are never one-size-fits-all. We design our healthcare revenue cycle management solutions with your unique needs in mind to improve efficiency and patient experience.
The Perfect Combination of Human Touch and Intelligent Tech Simplifies and Supercharges Your Revenue Cycle
We are a technology-powered, data-driven partner that will deliver exceptional results while maintaining excellent patient experience. We leverage a differentiating combination of AI and robotics powered tools and human expertise and service to solve our partners’ most complex RCM challenges. Put our 20+ years of experience and cutting-edge technology to improve your organization’s cash flow.

Tailored Solutions for Your Unique Revenue Cycle
Our solutions are never one-size-fits all. We work with your team to determine whether your organization would benefit from end-to-end revenue cycle management or if a more targeted solution would better address your revenue cycle needs.
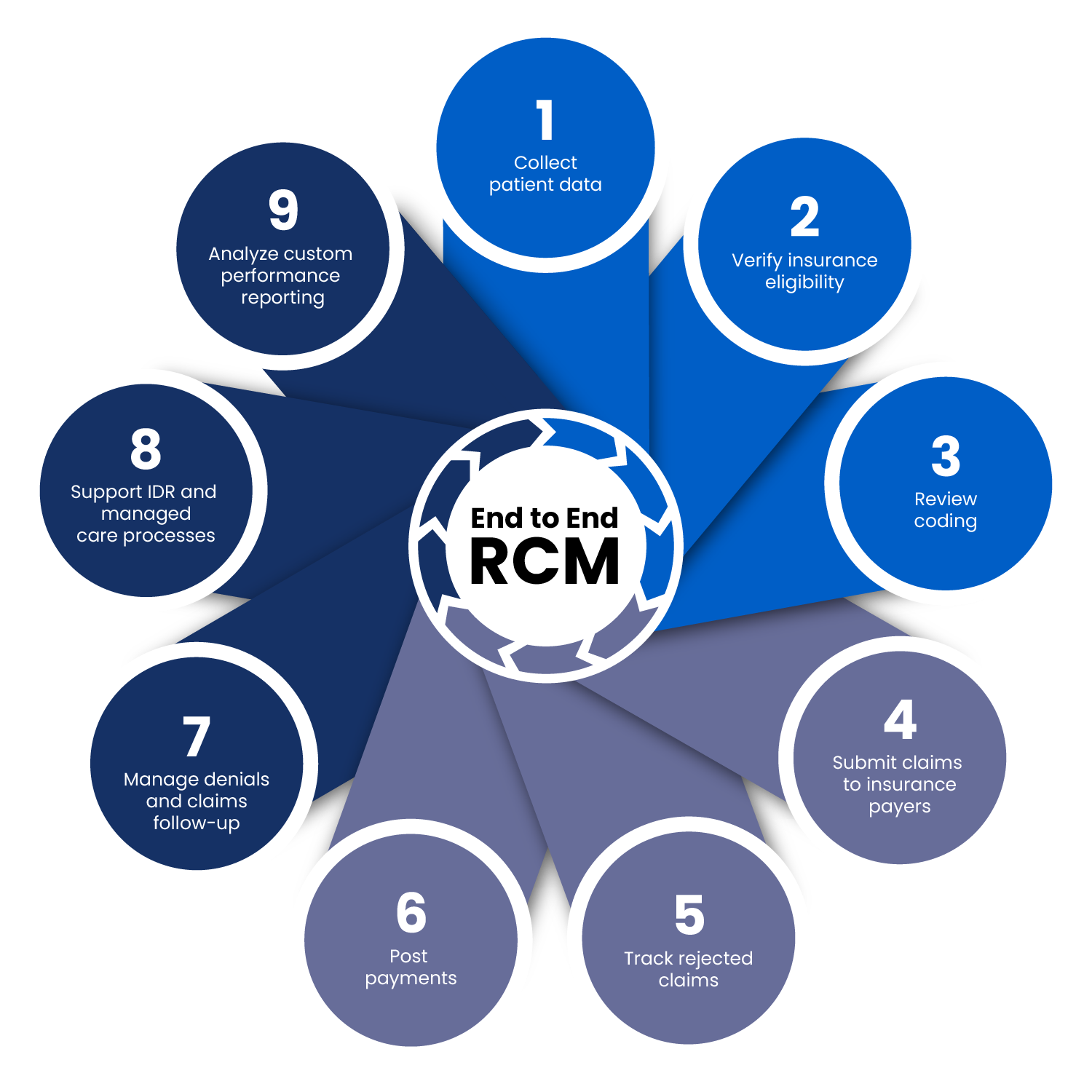
End-to-End RCM
We handle every aspect of your revenue cycle. From patient data collection to independent dispute resolution (IDR) and managed care processes, our experts optimize RCM.
Custom Solutions
Whatever your RCM challenge, we can develop a custom solution to help. In addition to our end-to-end RCM platform, we offer custom RCM solutions.
Our Partners Enjoy
%
clean claim rate
%
improvement in collections
%
reduction in RCM costs

Custom Solutions
We approach RCM differently, which means we skip anecdotal findings and get straight to meaningful ways to improve your billing and collections processes. Consistently, we find clear opportunities for RCM optimization that significantly boosts financial performance.
Below are some examples of custom solutions we provide. Contact us to discuss how you can mix and match services like the examples below to build an RCM solution that works for you.
Flexible RCM Services
Coding
Experience less denials and more revenue with our team of CPC professional coders.
- All charts are coded within 4 business days
- Performed by CPC-certified coders
- 10%+ of coded charts are audited
Arietis partners enjoy <1% coding-related rejections
Billing
We transmit 98.2% of our claims electronically and our precise processes systemically identify and prevent denials.
- Electronic claims submission
- Denial and appeals follow up within 10 days
- Full-service payer enrollment and payment posting
Arietis partners enjoy a 99.48% clean claim rate
Patient Engagement & 24/7 Call Center
Ensure optimal patient experience with our call center and full-service patient engagement tools.
- Full-service 24/7 patient support call center
- Easy-to-access electronic patient payment portal
- Patient-friendly statements, payment plans, and digital payment options
Arietis partners enjoy a <1.5% call center call abandonment rate
AR Management & Aging AR Resolution
Recover valuable AR with our unique claims resolution technology.
- Claims and accounts receivable follow up
- Claims disputes within 10 days
- Underpayment appeals within 30 days
Arietis partners enjoy 38 average days in AR
Worker's Comp & Auto Claims Management
Ensure all your providers are enrolled with the Department of Labor and ensure compliance with state mandated fee schedules.
- Connections with 85% of the nation’s largest carriers
- Electronic submission of worker’s compensation and auto claims
- Underpayment appeals
Arietis partners enjoy 95% adjudication rate of worker’s comp and auto claims
IDR & Managed Care Advisory Services
We develop custom consulting service engagements that delve deep into specific aspects of healthcare RCM.
- Managed care strategy to obtain optimal payer contracts
- IDR process support
- Conversion from outsourced to in-house billing support
Arietis partners enjoy a 15% improvement in collections on average
“Every time Arietis finds an opportunity to improve our RCM, they structure a solution. When they find an issue, they don’t just work the single claim, they solve the problem across all accounts.”
Garrison Gordon,
Director of Revenue Cycle Analytics
LET’S DISCUSS HOW WE CAN SUPPORT YOUR ORGANIZATION